

Jaundice – the disease we associate with the yellowing of the skin, doesn’t just affect adults. It is one of the many conditions a newborn can suffer from. Studies reveal that 6 out of every 10 babies are affected by jaundice, out of which 8 out of 10 are born prematurely.
The condition when a baby’s skin and eyes develop a yellowish color is called newborn jaundice. This is a very common occurrence in babies and is because of a high level of bilirubin present, which is a yellow pigment that is produced during a normal breakdown of red blood cells.
The liver processes bilirubin in older babies and adults, however, this is not the case in a newborn as the liver is not mature enough to filter out the bilirubin.
The good side to it is, in most cases, jaundice fades away as the baby develops and starts to feed which is helpful for the bilirubin to pass through the body and hence can be a very mild event
Mostly the jaundice cures within 2 to 3 weeks. If jaundice persists any longer than 3 weeks, it most probably can be due to an underlying condition.
Some of the repercussions of high Bilirubin levels are deafness, cerebral palsy, and other forms of brain damage.
What reasons could there be, for jaundice in newborns?
Most healthy babies tend to be affected by normal jaundice. This is because newborns have more blood cells than an adult. Since these blood cells don’t live as long, more bilirubin is formed when these break down.
In cases where the blood group of the newborn and the mother isn’t compatible, antibodies can develop in the baby that can destroy their red blood cells and hence lead to a sudden rise in the bilirubin levels.
Some other causes of neonatal jaundice include:
What symptoms should be focussed on, in cases of newborn jaundice?
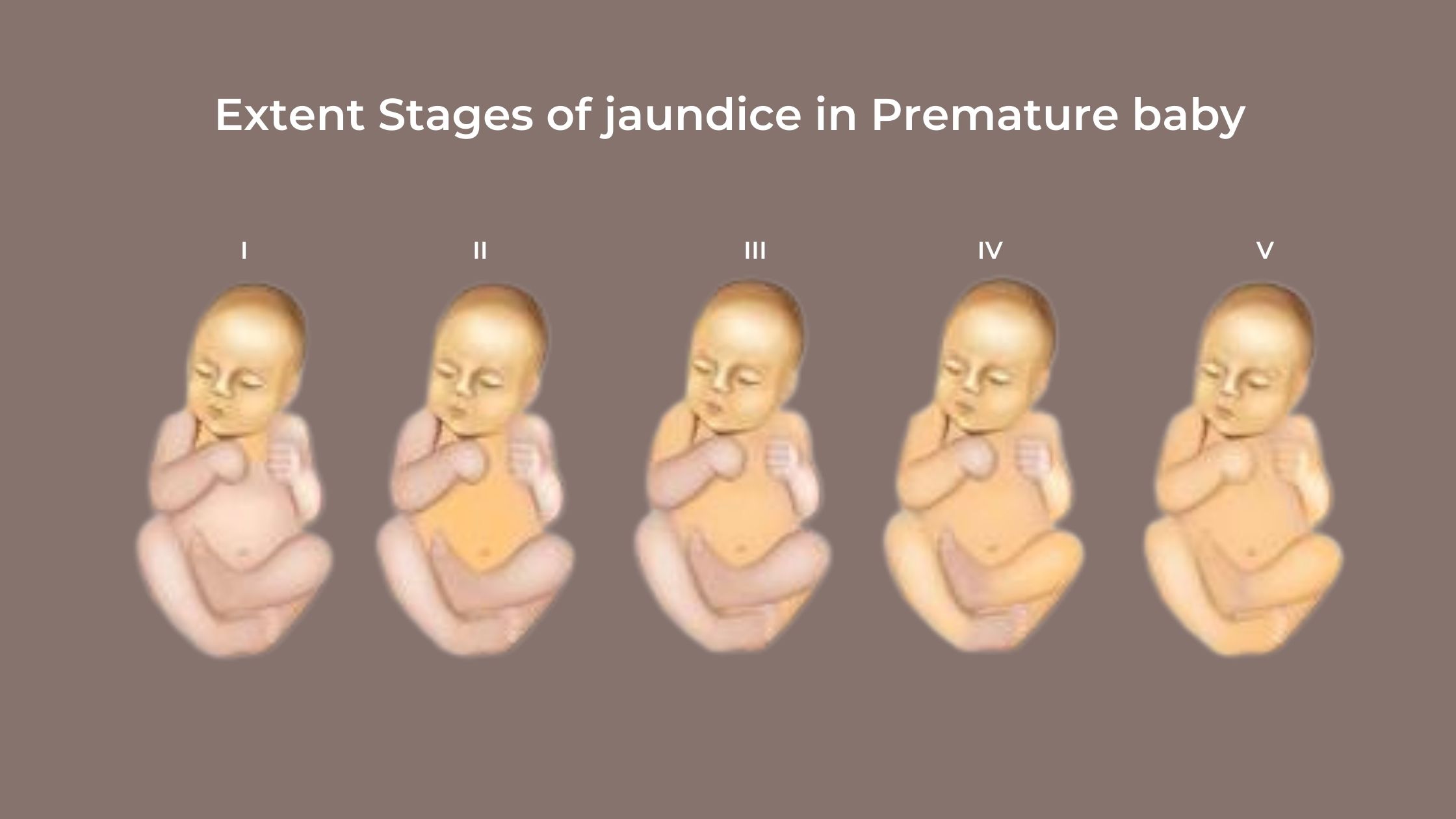
Look out for the whites of the eyes and the skin turning yellow. This usually appears between the second and the fourth-day post-birth. The yellowing begins to show up first on the face, followed by the chest and the legs. Babies with very high levels of bilirubin may be sleepy, fussy, and floppy. It is difficult to spot jaundice in darker complexioned babies, hence it is necessary to look out for other symptoms in this case.
To check if your baby has jaundice here is something you can try. Press lightly on your infant’s forehead or nose. If the skin looks yellowish on the area where you pressed, the baby likely has jaundice otherwise the skin color on that spot should look lighter than the normal color for a moment.
It is recommended to try doing this in good lighting conditions, during natural daylight.
Contact your doctor if:
What are the risk factors?
There are major risk factors for neonatal jaundice that can cause complications, they include but are not limited to.
Do not wait to get in touch with the doctor. Call them right away, if jaundice doesn’t seem to subside. Babies who have had jaundice for beyond 2 weeks need to undergo more testing to rule out any underlying reasons causing jaundice. There could be any problems with the liver or their bile system, their metabolism, or even their genes. Certain treatments include –
Newborns need constant care and support and in this case, do not hesitate to get medical intervention, as a stitch in time, saves nine. In this case, it can save a life.
Also Read: Stomach Worms in Children
Disclaimer: The information included here is only for knowledge sharing purposes, and the blog is not intended to be a substitute for diagnosis, medical advice, or treatment by a healthcare professional. Because individual needs appropriate advice, the reader should consult their doctor to determine the appropriate disease depending on their situation.


 Emergency Number
Emergency Number